The intricate ecosystem residing within the female reproductive tract represents one of the most fascinating and clinically significant microbial communities in the human body. The vaginal microbiome, composed of diverse bacterial species that maintain a delicate balance crucial for reproductive health, has emerged as a critical factor influencing fertility, conception success, and pregnancy outcomes. Recent advances in microbiome research have revealed that this microscopic world plays a far more substantial role in reproductive health than previously understood, extending its influence from the initial stages of conception through the complex journey of pregnancy and childbirth.
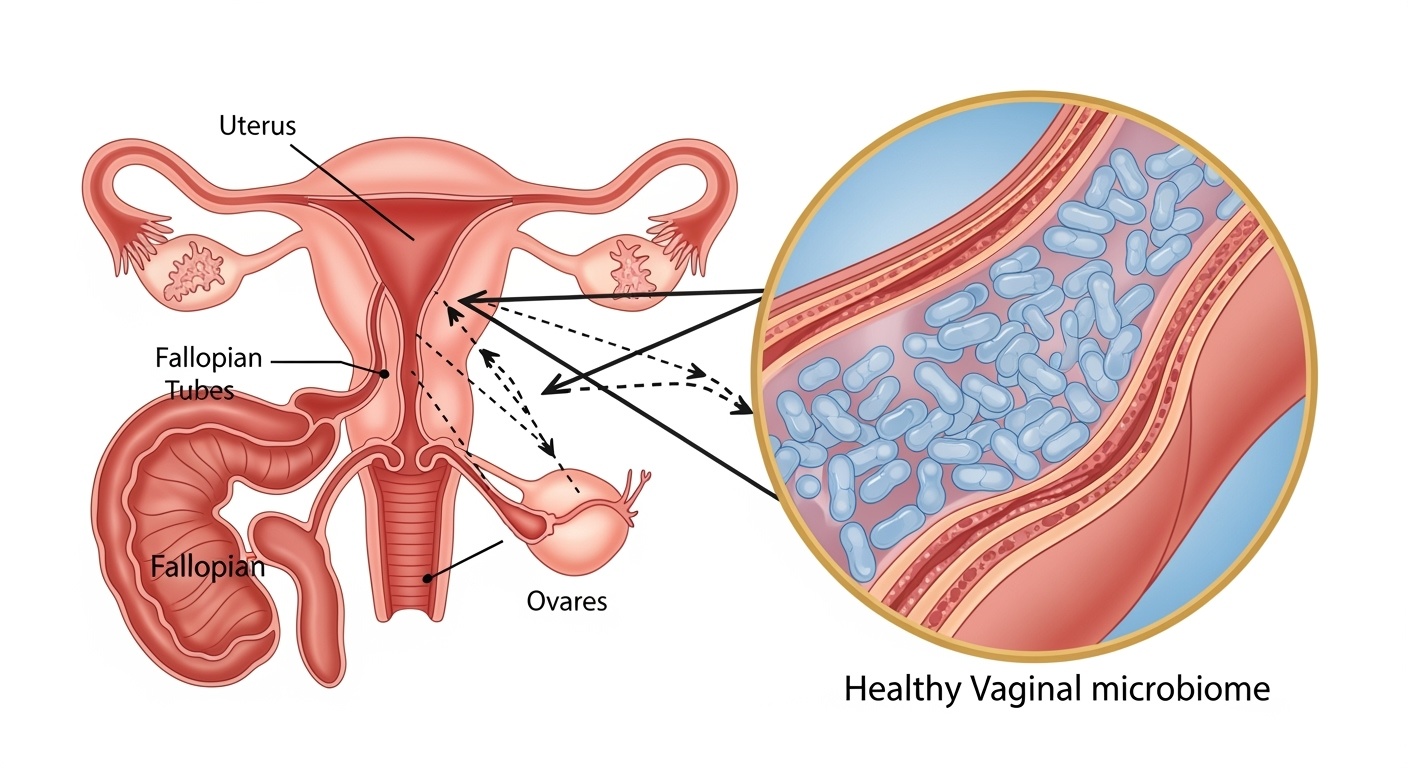
Understanding the vaginal microbiome requires appreciation of its unique characteristics that distinguish it from other body site microbiomes. Unlike the gut microbiome, which thrives on diversity, the healthy vaginal microbiome is characterized by low diversity and dominance by specific bacterial species, primarily Lactobacillus. This apparent simplicity masks a sophisticated biological system that has evolved to create optimal conditions for reproductive success while providing robust defense against pathogenic microorganisms that could compromise fertility and pregnancy health.
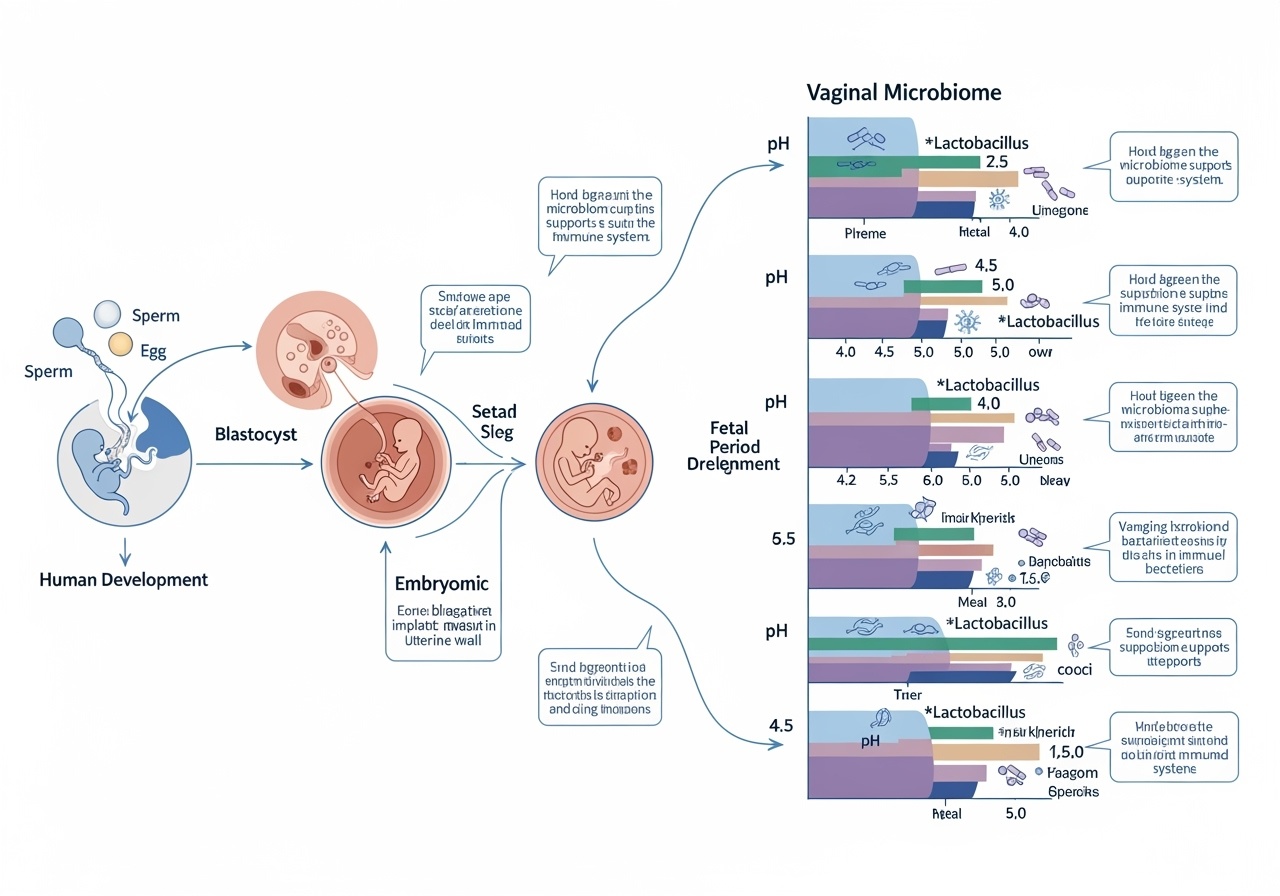
The relationship between the vaginal microbiome and reproductive outcomes operates through multiple interconnected mechanisms that influence every stage of the reproductive process. From creating an environment conducive to sperm survival and transport, to facilitating successful embryo implantation, to maintaining pregnancy stability and influencing birth outcomes, the microbiome serves as both guardian and facilitator of reproductive success. This comprehensive exploration reveals how understanding and optimizing the vaginal microbiome can significantly impact fertility outcomes and pregnancy health.
The Architecture of Reproductive Microbial Ecosystems
The vaginal microbiome exists as a dynamic ecosystem that varies significantly among individuals and populations, yet maintains consistent patterns that correlate with reproductive health outcomes. The predominant bacterial species, Lactobacillus, encompasses several distinct species including L. crispatus, L. gasseri, L. iners, and L. jensenii, each contributing unique metabolic capabilities and protective functions. These bacteria produce lactic acid through fermentation of glycogen deposits, creating an acidic environment with pH levels typically ranging from 3.8 to 4.5, which serves as the primary defense mechanism against pathogenic colonization.
The metabolic activity of Lactobacillus species extends beyond simple acid production to include synthesis of antimicrobial compounds such as bacteriocins, hydrogen peroxide, and biosurfactants that actively inhibit growth of potentially harmful microorganisms. This biochemical arsenal creates a protective barrier that prevents ascending infections that could compromise fertility by damaging reproductive organs or disrupting the delicate hormonal balance necessary for successful reproduction.
However, the vaginal microbiome is not uniformly dominated by Lactobacillus across all individuals. Research has identified distinct community state types that represent different stable configurations of the vaginal microbiome. While Lactobacillus-dominated communities are generally associated with optimal reproductive health, some individuals maintain healthy reproductive function with more diverse microbial communities. Understanding these variations is crucial for developing personalized approaches to reproductive health optimization.
The temporal dynamics of the vaginal microbiome reveal additional layers of complexity. Hormonal fluctuations throughout the menstrual cycle create cyclical changes in the microbial community composition and metabolic activity. Estrogen levels directly influence glycogen deposition in vaginal epithelial cells, which serves as the primary nutrient source for Lactobacillus species. This hormonal regulation creates a feedback loop where reproductive hormones shape the microbiome, while the microbiome influences local immune responses and hormone metabolism.
Microbiome-Mediated Mechanisms of Fertility Enhancement
The influence of the vaginal microbiome on fertility operates through multiple sophisticated mechanisms that begin with the initial encounter between sperm and the female reproductive tract. Upon ejaculation, sperm must navigate through the vaginal environment, and the composition of the local microbiome significantly impacts their survival, motility, and capacitation. A healthy, Lactobacillus-dominated microbiome creates optimal conditions for sperm function through maintenance of appropriate pH levels and production of metabolites that support sperm viability.
Research has revealed that specific bacterial species can either enhance or impair sperm function through direct interactions and indirect effects on the vaginal environment. Lactobacillus species produce metabolites that can improve sperm motility and reduce oxidative stress, while potentially harmful bacteria such as Gardnerella vaginalis and Atopobium vaginae can impair sperm function through production of toxic compounds and disruption of the optimal vaginal pH.
The microbiome’s influence extends beyond sperm survival to affect the complex process of fertilization itself. The ascension of sperm through the female reproductive tract requires coordinated interactions between sperm, cervical mucus, and the local microbial environment. Dysbiotic microbial communities can alter cervical mucus composition and create inflammatory conditions that impede sperm transport and reduce fertilization rates.
Furthermore, the vaginal microbiome influences ovarian function and egg quality through systemic and local immune modulation. Chronic inflammation associated with vaginal dysbiosis can affect hypothalamic-pituitary-ovarian axis function, potentially disrupting ovulation and compromising egg quality. The microbiome also influences local immune responses in the reproductive tract, which play crucial roles in creating an environment conducive to conception.
The relationship between the vaginal microbiome and assisted reproductive technologies has become increasingly recognized as a critical factor in treatment success. Studies have demonstrated that women with Lactobacillus-dominated vaginal microbiomes have significantly higher success rates with in vitro fertilization procedures compared to those with dysbiotic microbial communities. This finding has led to growing interest in microbiome optimization as an adjunctive treatment for infertility.
The Pregnancy Microbiome Continuum
The transition from conception to pregnancy brings profound changes in the vaginal microbiome that reflect the complex physiological adaptations necessary for successful pregnancy maintenance. These changes begin immediately following conception and continue throughout pregnancy, with the microbiome playing active roles in implantation, placental development, and pregnancy maintenance. Understanding these dynamic changes provides insights into how microbiome health influences pregnancy outcomes and reveals opportunities for intervention to improve reproductive success.
During early pregnancy, hormonal changes create an environment that favors specific microbial communities while suppressing others. The dramatic increase in estrogen and progesterone levels leads to increased glycogen deposition and altered immune responses that shape the microbial landscape. These changes generally favor Lactobacillus dominance, creating conditions that support embryo implantation and early placental development.
The process of embryo implantation requires precise coordination between maternal immune responses and the developing embryo. The vaginal microbiome influences this process through modulation of local and systemic immune function. A healthy microbiome promotes appropriate immune tolerance that allows successful embryo implantation while maintaining protective responses against potential pathogens. Dysbiotic microbial communities can create inflammatory conditions that impair implantation success and increase risk of early pregnancy loss.
As pregnancy progresses, the vaginal microbiome continues to evolve in response to changing hormonal levels and physiological demands. The microbiome becomes increasingly stable and Lactobacillus-dominated, reaching maximum stability during the second trimester. This stability is thought to reflect the body’s preparation for the vulnerable period of late pregnancy when ascending infections pose the greatest risk to pregnancy outcomes.
The relationship between the vaginal microbiome and pregnancy complications reveals the clinical significance of maintaining optimal microbial health throughout pregnancy. Bacterial vaginosis, characterized by loss of Lactobacillus dominance and overgrowth of anaerobic bacteria, is associated with increased risk of preterm birth, low birth weight, and other adverse pregnancy outcomes. These associations highlight the importance of monitoring and maintaining vaginal microbiome health throughout pregnancy.
Dysbiosis and Reproductive Pathology
Vaginal dysbiosis, characterized by disruption of the normal Lactobacillus-dominated microbial community, represents a significant threat to reproductive health that can manifest through various pathological conditions and adverse outcomes. The transition from a healthy, balanced microbiome to a dysbiotic state involves complex interactions between host factors, environmental influences, and microbial dynamics that can have profound implications for fertility and pregnancy success.
Bacterial vaginosis represents the most common form of vaginal dysbiosis, affecting up to 30% of reproductive-age women. This condition is characterized by overgrowth of anaerobic bacteria including Gardnerella vaginalis, Atopobium vaginae, and various Bacteroides species, accompanied by a significant reduction in Lactobacillus populations. The metabolic activities of these bacteria create an alkaline environment that disrupts normal vaginal physiology and compromises the protective functions of the healthy microbiome.
The impact of bacterial vaginosis on fertility extends beyond the immediate vaginal environment to affect multiple aspects of reproductive function. Women with bacterial vaginosis experience increased rates of pelvic inflammatory disease, which can lead to fallopian tube damage and increased risk of ectopic pregnancy. The inflammatory cytokines produced in response to dysbiotic bacteria can also affect ovarian function and disrupt the delicate hormonal balance necessary for successful reproduction.
Recurrent bacterial vaginosis presents particular challenges for reproductive health, as repeated episodes of dysbiosis can cause cumulative damage to the reproductive tract and establish persistent inflammatory states that compromise fertility. The biofilm-forming capabilities of many dysbiosis-associated bacteria contribute to treatment resistance and recurrence, creating chronic conditions that require comprehensive management approaches.
The relationship between vaginal dysbiosis and sexually transmitted infections creates additional layers of complexity in reproductive health management. Dysbiotic microbial communities increase susceptibility to viral, bacterial, and parasitic sexually transmitted infections that can have serious consequences for fertility and pregnancy outcomes. The loss of Lactobacillus-mediated protection allows opportunistic pathogens to establish infection and potentially cause permanent damage to reproductive organs.
Emerging research has revealed connections between vaginal dysbiosis and systemic health conditions that affect reproduction. Women with bacterial vaginosis have increased rates of insulin resistance, metabolic syndrome, and chronic inflammatory conditions that can impact fertility through multiple pathways. These findings suggest that vaginal microbiome health may serve as both a marker and mediator of overall reproductive health status.
Hormonal Orchestration of Microbial Communities
The intricate relationship between reproductive hormones and the vaginal microbiome represents one of the most sophisticated examples of host-microbe coevolution in human biology. This bidirectional communication system allows hormonal fluctuations to shape microbial communities while enabling the microbiome to influence hormone metabolism and activity. Understanding these interactions provides crucial insights into how hormonal health affects reproductive outcomes through microbiome-mediated mechanisms.
Estrogen serves as the primary hormonal regulator of vaginal microbiome composition through its effects on vaginal epithelial cells. Estrogen stimulates glycogen synthesis and deposition in vaginal epithelial cells, creating the primary nutrient source for Lactobacillus species. This mechanism explains why estrogen deficiency states, such as menopause or certain reproductive disorders, are associated with loss of Lactobacillus dominance and increased susceptibility to vaginal dysbiosis.
The cyclical nature of estrogen production throughout the menstrual cycle creates corresponding fluctuations in vaginal microbiome composition and activity. During the follicular phase, rising estrogen levels promote Lactobacillus growth and acid production, creating optimal conditions for sperm survival and transport. The luteal phase brings changes in progesterone levels that can influence immune responses and microbial community dynamics, potentially affecting implantation success.
Progesterone influences the vaginal microbiome through both direct and indirect mechanisms. Direct effects include modulation of epithelial cell metabolism and immune cell function, while indirect effects occur through interactions with other hormonal systems. Progesterone’s immunomodulatory properties help maintain appropriate immune tolerance during pregnancy while preserving protective antimicrobial responses.
The microbiome reciprocally influences hormone metabolism through bacterial enzyme systems that can metabolize steroid hormones and produce hormone-like compounds. Certain bacterial species possess enzymes capable of converting inactive hormone precursors into active forms, while others can break down hormones and influence their local concentrations. These activities create feedback loops that can significantly impact reproductive physiology.
Disruptions in the hormone-microbiome axis can have cascading effects on reproductive health. Conditions such as polycystic ovary syndrome, which involve altered hormone production and metabolism, are associated with changes in vaginal microbiome composition that may contribute to reproductive dysfunction. Understanding these relationships opens new avenues for therapeutic intervention that target both hormonal and microbial components of reproductive health.
Nutritional Foundations of Microbiome Health
The composition and stability of the vaginal microbiome are profoundly influenced by nutritional factors that affect both systemic health and local microbial environment. Emerging research has revealed complex relationships between dietary patterns, nutrient availability, and vaginal microbiome health that have significant implications for reproductive outcomes. Understanding these nutritional foundations provides opportunities for evidence-based interventions to optimize microbiome health and enhance fertility.
Dietary patterns that promote systemic health also tend to support optimal vaginal microbiome composition. Mediterranean-style diets rich in fruits, vegetables, whole grains, and healthy fats are associated with increased Lactobacillus dominance and reduced risk of bacterial vaginosis. These dietary patterns provide antioxidants, anti-inflammatory compounds, and prebiotic fibers that support beneficial bacteria while creating conditions unfavorable for pathogenic microorganisms.
The role of specific nutrients in supporting vaginal microbiome health has become an area of intensive research interest. Vitamin D deficiency has been associated with increased risk of bacterial vaginosis and reduced Lactobacillus populations, likely through effects on immune function and antimicrobial peptide production. Adequate vitamin D status appears necessary for maintaining the immune responses that support healthy microbial communities.
Omega-3 fatty acids demonstrate significant potential for supporting vaginal microbiome health through their anti-inflammatory properties and effects on bacterial membrane composition. Women consuming higher levels of omega-3 fatty acids show increased stability of Lactobacillus-dominated communities and reduced rates of dysbiosis-related complications. These effects may occur through modulation of local inflammatory responses and direct effects on bacterial growth and metabolism.
The gut-vaginal microbiome axis represents an important pathway through which nutrition influences reproductive health. Dietary fibers that support beneficial gut bacteria can indirectly influence vaginal microbiome composition through systemic immune modulation and production of metabolites that affect microbial communities throughout the body. This connection explains how comprehensive nutritional approaches that support overall microbial health can have specific benefits for reproductive outcomes.
Probiotics represent a direct nutritional intervention for vaginal microbiome optimization, though their effects vary significantly depending on bacterial strains, dosing regimens, and individual factors. Lactobacillus probiotics specifically designed for vaginal health have shown promise in restoring healthy microbial communities and preventing recurrent dysbiosis. However, successful probiotic interventions require careful selection of appropriate strains and consideration of individual microbiome characteristics.
| Nutritional Factor | Mechanism of Action | Impact on Microbiome | Reproductive Benefits |
| Vitamin D | Immune modulation, antimicrobial peptide production | Supports Lactobacillus dominance | Reduced BV risk, improved conception rates |
| Omega-3 Fatty Acids | Anti-inflammatory, membrane stabilization | Increased microbiome stability | Enhanced fertility, reduced pregnancy complications |
| Prebiotic Fibers | Selective bacterial nutrition | Promotes beneficial bacteria growth | Improved vaginal pH, reduced dysbiosis |
| Antioxidants | Oxidative stress reduction | Protects beneficial bacteria | Enhanced sperm survival, improved egg quality |
Environmental and Lifestyle Determinants
The vaginal microbiome exists within a complex web of environmental and lifestyle influences that can significantly impact its composition, stability, and function. Understanding these determinants is crucial for developing comprehensive approaches to reproductive health optimization that address the multiple factors contributing to microbiome health. Modern lifestyle factors present both challenges and opportunities for maintaining optimal microbial communities that support reproductive success.
Antibiotic exposure represents one of the most significant environmental threats to vaginal microbiome health. While antibiotics can be life-saving medications, their broad-spectrum antimicrobial effects often disrupt healthy microbial communities along with pathogenic bacteria. Women who receive antibiotic treatment frequently experience loss of Lactobacillus dominance and subsequent overgrowth of opportunistic bacteria, leading to bacterial vaginosis and associated reproductive complications.
The timing of antibiotic exposure relative to conception attempts and pregnancy can have particularly significant implications. Antibiotic-induced dysbiosis during critical reproductive windows may impair fertility and increase risk of pregnancy complications. However, the effects of antibiotics on the vaginal microbiome are not permanent, and targeted interventions can help restore healthy microbial communities following antibiotic treatment.
Stress represents another major lifestyle factor that influences vaginal microbiome health through multiple pathways. Chronic psychological stress affects immune function, hormone production, and inflammation levels, all of which can alter microbial community composition. Stress-induced changes in cortisol levels can suppress immune responses that normally maintain healthy microbial balance, leading to increased susceptibility to dysbiosis and associated reproductive problems.
Sexual activity and practices significantly influence vaginal microbiome composition through introduction of new microorganisms, changes in pH, and alterations in the vaginal environment. While sexual activity is a normal and healthy aspect of reproductive life, certain practices can increase risk of microbial disruption. Understanding these relationships allows for development of strategies that maintain sexual health while preserving optimal microbiome conditions.
Hygiene practices represent a modifiable lifestyle factor that can significantly impact vaginal microbiome health. Excessive or inappropriate cleaning products, douching, and certain feminine hygiene products can disrupt the natural microbial balance and compromise protective mechanisms. Evidence-based hygiene recommendations that preserve natural microbial communities while maintaining cleanliness are essential for optimal reproductive health.
Sleep quality and circadian rhythm disruption have emerged as important factors influencing microbiome health throughout the body, including the vaginal microbiome. Irregular sleep patterns and poor sleep quality can affect immune function, hormone production, and stress responses that influence microbial community stability. Optimizing sleep hygiene may therefore represent an important component of comprehensive reproductive health strategies.
Clinical Assessment and Microbiome Testing
The clinical evaluation of vaginal microbiome health has evolved significantly with advances in molecular diagnostic techniques and growing understanding of the relationship between microbial communities and reproductive outcomes. Modern assessment approaches combine traditional clinical evaluation with sophisticated laboratory testing to provide comprehensive insights into microbiome composition, function, and health implications. Understanding these assessment methods is crucial for healthcare providers and individuals seeking to optimize their reproductive health.
Traditional clinical assessment of vaginal health relies on microscopic examination of vaginal secretions, pH measurement, and evaluation of symptoms and physical findings. While these methods remain valuable for diagnosing obvious pathological conditions such as bacterial vaginosis and yeast infections, they provide limited information about the complex microbial ecosystems that influence reproductive health. The subjective nature of symptom assessment and the limitations of microscopic examination can lead to underdiagnosis of subtle dysbiotic conditions that may impact fertility.
Molecular diagnostic techniques have revolutionized the assessment of vaginal microbiome health by providing detailed information about microbial community composition and abundance. Quantitative polymerase chain reaction testing allows for precise measurement of specific bacterial species, including the various Lactobacillus species that are crucial for reproductive health. This technology can detect low levels of pathogenic bacteria that may not be visible through traditional microscopic methods.
Next-generation sequencing represents the most comprehensive approach to vaginal microbiome assessment, providing detailed profiles of entire microbial communities including rare and previously uncharacterized species. This technology reveals the complex ecological relationships within vaginal microbial communities and can identify subtle imbalances that may affect reproductive outcomes. However, the interpretation of sequencing results requires sophisticated bioinformatics analysis and clinical expertise.
The development of clinically relevant biomarkers for vaginal microbiome health has focused on identifying specific bacterial ratios, metabolite profiles, and immune markers that correlate with reproductive outcomes. The Lactobacillus-to-anaerobe ratio has emerged as a useful indicator of microbiome health, while inflammatory markers such as interleukin-1β and tumor necrosis factor-α can indicate dysbiosis-associated inflammation that may impact fertility.
Functional assessment of the vaginal microbiome extends beyond simple compositional analysis to evaluate the metabolic activities and protective functions of microbial communities. Measurement of lactic acid production, antimicrobial peptide levels, and pH stability provides insights into the functional capacity of the microbiome to support reproductive health. These functional assessments can reveal microbiome dysfunction even when compositional analysis appears normal.
| Assessment Method | Information Provided | Clinical Applications | Limitations |
| Traditional Microscopy | Basic bacterial morphology, inflammatory cells | Diagnosis of obvious infections | Limited sensitivity, subjective interpretation |
| qPCR Testing | Specific bacterial quantification | Targeted pathogen detection | Limited scope, expensive |
| Next-Generation Sequencing | Comprehensive community profiling | Research applications, detailed analysis | Complex interpretation, high cost |
| Biomarker Assessment | Functional indicators, inflammatory status | Clinical monitoring, treatment response | Emerging field, limited validation |
Therapeutic Interventions and Microbiome Restoration
The restoration of healthy vaginal microbiome communities following dysbiosis represents a critical component of comprehensive reproductive health management. Therapeutic interventions for microbiome restoration must address both the elimination of harmful microorganisms and the reestablishment of beneficial bacterial populations that support reproductive function. Understanding the various therapeutic approaches and their mechanisms of action is essential for developing effective treatment strategies that optimize reproductive outcomes.
Conventional antimicrobial therapy remains the first-line treatment for bacterial vaginosis and other forms of vaginal dysbiosis, though its limitations have become increasingly apparent. Metronidazole and clindamycin, the most commonly prescribed antibiotics for bacterial vaginosis, effectively eliminate anaerobic bacteria responsible for dysbiotic conditions but often fail to restore Lactobacillus dominance. This incomplete restoration frequently leads to recurrent dysbiosis and persistent reproductive health problems.
The development of targeted antimicrobial approaches that selectively eliminate pathogenic bacteria while preserving beneficial species represents an important advancement in microbiome-based therapeutics. Narrow-spectrum antimicrobials, antimicrobial peptides, and bacteriophage therapy offer promising alternatives to broad-spectrum antibiotics that can cause collateral damage to healthy microbial communities. These targeted approaches may improve treatment outcomes while reducing the risk of recurrent dysbiosis.
Probiotic therapy has emerged as a cornerstone of microbiome restoration strategies, though success depends critically on strain selection, formulation, and dosing protocols. Lactobacillus probiotics specifically selected for vaginal health applications have demonstrated efficacy in restoring healthy microbial communities and maintaining long-term microbiome stability. However, not all probiotic strains are equally effective, and individual responses can vary significantly based on host factors and existing microbiome composition.
The timing and duration of probiotic therapy significantly influence treatment outcomes. Concurrent administration of probiotics with antimicrobial therapy can help prevent dysbiosis and accelerate microbiome restoration, while extended probiotic courses may be necessary to establish stable beneficial bacterial populations. Personalized probiotic protocols based on individual microbiome assessment may optimize treatment efficacy and reduce recurrence rates.
Prebiotic interventions that support the growth and activity of beneficial bacteria represent an important complementary approach to microbiome restoration. Vaginal prebiotics can provide selective nutrition for Lactobacillus species while creating conditions unfavorable for pathogenic bacteria. These interventions may be particularly valuable for maintaining long-term microbiome stability following successful restoration therapy.
Combination therapies that integrate antimicrobial treatment, probiotic restoration, and prebiotic support offer the potential for more comprehensive and durable microbiome restoration. These multimodal approaches address the complex ecological factors that contribute to dysbiosis while supporting the reestablishment of healthy microbial communities. Early evidence suggests that combination therapies may achieve higher cure rates and lower recurrence rates compared to single-agent treatments.
Reproductive Technology and Microbiome Optimization
The integration of microbiome optimization into assisted reproductive technology protocols represents a rapidly evolving field that has the potential to significantly improve treatment outcomes for couples struggling with infertility. As understanding of the relationship between vaginal microbiome health and reproductive success has grown, fertility clinics have begun incorporating microbiome assessment and optimization into their treatment protocols. This integration requires careful consideration of the timing, methods, and expected outcomes of microbiome interventions in the context of assisted reproduction.
The impact of vaginal microbiome composition on in vitro fertilization success rates has been documented through multiple studies demonstrating significantly higher pregnancy rates among women with Lactobacillus-dominated microbial communities. These findings have led to growing interest in pretreatment microbiome optimization as a strategy for improving IVF outcomes. However, the optimal timing and methods for microbiome intervention in the context of IVF treatment remain areas of active research and clinical development.
Embryo transfer procedures present a critical window during which vaginal microbiome composition may influence implantation success. The presence of pathogenic bacteria or inflammatory conditions associated with dysbiosis can create an environment hostile to embryo implantation and early pregnancy development. Some fertility clinics have begun screening for vaginal dysbiosis prior to embryo transfer and treating identified imbalances to optimize implantation conditions.
The influence of the endometrial microbiome on assisted reproductive technology outcomes has emerged as another important consideration in fertility treatment protocols. While the endometrial microbiome is distinct from the vaginal microbiome, these communities are interconnected and can influence each other through ascending bacterial migration and systemic immune effects. Understanding these relationships is crucial for developing comprehensive microbiome optimization strategies for fertility treatment.
Personalized microbiome interventions based on individual microbial profiles represent the future direction of fertility treatment optimization. Advanced diagnostic techniques that characterize both vaginal and endometrial microbiome composition can guide targeted interventions that address specific imbalances and optimize conditions for reproductive success. These personalized approaches may significantly improve treatment outcomes while reducing the time and cost associated with fertility treatments.
The development of microbiome-based biomarkers for predicting fertility treatment outcomes offers the potential for more precise treatment planning and patient counseling. Specific microbial signatures that correlate with treatment success could help identify patients who may benefit from additional interventions or alternative treatment approaches. These predictive tools may ultimately improve the efficiency and effectiveness of fertility treatments.
Pregnancy Outcomes and Microbial Influences
The relationship between vaginal microbiome health and pregnancy outcomes extends throughout the entire gestational period, influencing everything from early implantation success to birth complications and neonatal health. Understanding these relationships is crucial for developing comprehensive prenatal care strategies that optimize both maternal and fetal health through microbiome-mediated mechanisms. The evidence linking specific microbial patterns to pregnancy outcomes continues to grow, providing new opportunities for interventions that improve reproductive success.
Preterm birth represents one of the most significant pregnancy complications associated with vaginal dysbiosis, affecting approximately 10% of pregnancies and contributing to substantial neonatal morbidity and mortality. Bacterial vaginosis and other forms of vaginal dysbiosis are associated with two to three-fold increases in preterm birth risk through mechanisms involving ascending infection, inflammation, and disruption of normal pregnancy maintenance pathways. Understanding these mechanisms has led to screening and treatment protocols aimed at reducing preterm birth risk through microbiome optimization.
The pathophysiology of dysbiosis-associated preterm birth involves complex interactions between pathogenic bacteria, host immune responses, and pregnancy-maintaining mechanisms. Bacterial products such as lipopolysaccharides and other inflammatory mediators can trigger prostaglandin production and cervical ripening that leads to premature labor initiation. Additionally, bacterial enzymes can break down protective cervical mucus and compromise the mechanical barriers that normally prevent ascending infection.
Low birth weight represents another significant pregnancy outcome influenced by maternal microbiome health. Women with vaginal dysbiosis experience increased rates of intrauterine growth restriction and small-for-gestational-age infants, likely through inflammatory mechanisms that affect placental function and fetal development. These effects highlight the importance of maintaining optimal microbiome health throughout pregnancy to support healthy fetal growth and development.
The timing of microbiome interventions during pregnancy requires careful consideration of both efficacy and safety. While treatment of symptomatic vaginal infections is clearly indicated, the optimal approach to asymptomatic dysbiosis during pregnancy remains controversial. Some studies suggest that early pregnancy treatment of bacterial vaginosis may reduce preterm birth risk, while others question the safety and efficacy of antimicrobial interventions during pregnancy.
The influence of maternal microbiome health on neonatal outcomes extends beyond birth weight and gestational age to include effects on early immune system development and long-term health outcomes. The process of birth through the vaginal canal exposes newborns to maternal microbial communities that play crucial roles in establishing the infant microbiome and immune system development. Disruptions in maternal microbiome health can therefore have lasting effects on child health and development.
| Pregnancy Outcome | Associated Microbiome Pattern | Risk Magnitude | Proposed Mechanism |
| Preterm Birth | Bacterial vaginosis, Gardnerella dominance | 2-3 fold increase | Ascending infection, inflammatory cascade |
| Low Birth Weight | Dysbiotic communities, reduced Lactobacillus | 1.5-2 fold increase | Placental inflammation, growth restriction |
| Pregnancy Loss | Pathogenic bacteria, immune dysregulation | Variable increase | Implantation failure, fetal rejection |
| Birth Complications | Chorioamnionitis-associated bacteria | Significant increase | Membrane rupture, infection |
Future Directions and Emerging Therapies
The rapidly evolving field of reproductive microbiome research continues to reveal new opportunities for therapeutic intervention and clinical application. Emerging technologies and therapeutic approaches promise to revolutionize the prevention and treatment of microbiome-related reproductive health problems while providing new insights into the fundamental mechanisms linking microbial communities to reproductive outcomes. Understanding these future directions is essential for healthcare providers and researchers working to optimize reproductive health through microbiome-based interventions.
Personalized microbiome medicine represents one of the most promising future directions in reproductive health, utilizing individual microbial profiles to guide targeted interventions and treatment selection. Advanced diagnostic techniques that combine microbiome sequencing with metabolomic analysis and immune profiling can provide comprehensive assessments of reproductive microbiome health that guide personalized treatment protocols. These approaches may significantly improve treatment outcomes while reducing adverse effects and treatment failures.
The development of next-generation probiotics specifically engineered for reproductive health applications offers exciting possibilities for microbiome restoration and optimization. These engineered probiotics may incorporate enhanced colonization capabilities, targeted antimicrobial properties, and improved stability characteristics that overcome limitations of traditional probiotic preparations. Additionally, synthetic biology approaches may enable the development of designer microorganisms that provide specific therapeutic functions tailored to individual patient needs.
Microbiome transplantation techniques, already successful in treating recurrent Clostridioides difficile infection, are being investigated for applications in reproductive health. Vaginal microbiome transplantation from healthy donors could potentially restore beneficial microbial communities in women with recurrent dysbiosis or treatment-resistant infections. However, significant safety and regulatory considerations must be addressed before these approaches can be implemented clinically.
The integration of artificial intelligence and machine learning technologies into microbiome research is accelerating the identification of novel therapeutic targets and predictive biomarkers. These computational approaches can analyze complex microbial datasets to identify patterns and relationships that may not be apparent through traditional analysis methods. Machine learning algorithms may ultimately enable real-time optimization of microbiome interventions based on individual patient characteristics and treatment responses.
Combination therapies that integrate microbiome interventions with traditional reproductive treatments represent another important area of development. These approaches may combine hormonal therapies, assisted reproductive technologies, and microbiome optimization strategies to achieve synergistic improvements in reproductive outcomes. Early evidence suggests that such integrated approaches may be more effective than individual interventions alone.
The expansion of microbiome research to include male reproductive health represents an important frontier that has been relatively underexplored. Understanding the role of male genital tract microbiomes in fertility and pregnancy outcomes may reveal new opportunities for couples-based interventions that optimize reproductive success through comprehensive microbiome management approaches.
Clinical Implementation and Patient Care
The translation of microbiome research findings into clinical practice requires careful consideration of practical implementation strategies, patient education approaches, and quality assurance measures that ensure safe and effective delivery of microbiome-based interventions. Healthcare providers must develop competencies in microbiome assessment and management while maintaining evidence-based approaches that prioritize patient safety and clinical efficacy. Understanding these implementation considerations is crucial for the successful integration of microbiome medicine into reproductive healthcare.
Patient education represents a critical component of successful microbiome-based interventions, as many individuals have limited understanding of the relationship between microbial communities and reproductive health. Educational approaches must communicate complex scientific concepts in accessible terms while providing practical guidance for lifestyle modifications and treatment adherence. Effective patient education can significantly improve treatment outcomes while empowering individuals to take active roles in optimizing their reproductive health.
The development of standardized protocols for microbiome assessment and intervention is essential for ensuring consistent and effective clinical care. These protocols must address appropriate indications for testing, interpretation of results, treatment selection criteria, and monitoring approaches that track treatment response and long-term outcomes. Standardization efforts should balance evidence-based medicine principles with flexibility to accommodate individual patient needs and preferences.
Quality assurance measures for microbiome testing and interventions must address the technical challenges associated with microbial analysis and the variability inherent in biological systems. Laboratory certification, proficiency testing, and result validation procedures are necessary to ensure accurate and reliable microbiome assessments. Additionally, product quality standards for probiotics and other microbiome-based therapeutics are essential for ensuring consistent therapeutic efficacy.
The integration of microbiome interventions into existing reproductive healthcare workflows requires consideration of cost-effectiveness, resource allocation, and provider training needs. Healthcare systems must evaluate the clinical and economic benefits of microbiome-based approaches while developing sustainable implementation strategies that can be maintained over time. These considerations may influence the adoption and dissemination of microbiome medicine in reproductive healthcare.
Ethical considerations surrounding microbiome medicine include issues of informed consent, privacy protection, and equitable access to emerging technologies. Patients must understand the limitations and uncertainties associated with microbiome interventions while being fully informed about potential risks and benefits. Additionally, efforts must be made to ensure that advances in microbiome medicine do not exacerbate existing healthcare disparities or create new barriers to reproductive healthcare access.
Conclusion and Future Perspectives
The vaginal microbiome has emerged as a critical determinant of reproductive health that influences every stage of the reproductive process from conception through pregnancy and birth. The complex relationships between microbial communities, host physiology, and reproductive outcomes reveal new opportunities for optimizing fertility and pregnancy success through evidence-based microbiome interventions. As our understanding of these relationships continues to evolve, the potential for microbiome-based approaches to transform reproductive healthcare becomes increasingly apparent.
The integration of microbiome science into reproductive medicine represents a paradigm shift toward more personalized and holistic approaches to fertility and pregnancy care. Rather than focusing solely on hormonal and structural aspects of reproduction, healthcare providers can now consider the microbial ecosystem as an active participant in reproductive success that can be assessed, monitored, and optimized. This expanded perspective opens new avenues for intervention while providing deeper insights into the mechanisms underlying reproductive health and disease.
The clinical applications of reproductive microbiome research continue to expand as diagnostic technologies improve and therapeutic interventions become more sophisticated. From screening and prevention strategies that identify and address microbiome imbalances before they impact fertility, to targeted treatments that restore healthy microbial communities and optimize pregnancy outcomes, microbiome-based approaches offer promising solutions to persistent reproductive health challenges.
However, significant challenges remain in translating microbiome research findings into widespread clinical practice. The complexity of microbial ecosystems, individual variation in microbiome composition and function, and the need for long-term safety and efficacy data all present obstacles that must be addressed through continued research and clinical development. Additionally, healthcare systems must develop the infrastructure and expertise necessary to implement microbiome-based interventions effectively and safely.
The future of reproductive microbiome medicine lies in the development of integrated approaches that combine advanced diagnostic capabilities with personalized therapeutic interventions tailored to individual patient needs and characteristics. As our understanding of host-microbe interactions continues to deepen and technological capabilities advance, the potential for microbiome-based approaches to improve reproductive outcomes and transform fertility care becomes increasingly promising.
The journey toward optimizing reproductive health through microbiome medicine represents an exciting frontier that promises to benefit countless individuals and couples struggling with fertility challenges. By recognizing the vaginal microbiome as a critical component of reproductive health and developing evidence-based strategies for its assessment and optimization, healthcare providers can offer new hope and improved outcomes for those seeking to achieve healthy pregnancies and successful reproductive outcomes.
 world
world
